

As published by CMS, these are the income limits for key coverage groups under Mississippi’s Medicaid program (note that these numbers include a built-in 5% income disregard that’s used for income-based Medicaid eligibility determinations):
Mississippi has not implemented Medicaid expansion under the ACA, so non-disabled adults without dependent children are not eligible for Medicaid regardless of how low their income is. Several Medicaid expansion bills were introduced in Mississippi’s legislature in 2024 to expand Medicaid under the ACA, including HB 1725. 3
That legislation passed in the Mississippi House in February, and the Senate passed a different version in March, with a stronger work requirement that would have made expansion largely unworkable. The two chambers were not able to reconcile their differences by the end of the session, and the measure died. 4 Lawmakers have said that Medicaid expansion is likely to be considered again in the 2025 legislative session. 5
of Federal Poverty Level
You can enroll through HealthCare.gov or you can fill out a PDF of the Mississippi Medicaid Application Form. You can also enroll by phone at 800-318-2596.
Eligibility: Parents with dependent children are eligible with household incomes up to 22% of FPL. Children are eligible for Medicaid or CHIP with household incomes up to 209% of FPL, and pregnant women are eligible with household incomes up to 194% of FPL.



Mississippi Medicaid has not been expanded as allowed under the Affordable Care Act (ACA), despite the state medical association’s support of expansion going back to August 2016.
Mississippi is one of just 10 states that have not yet expanded Medicaid as of 2024. As noted above, several bills to expand Medicaid were introduced in the 2024 session, and one of them — HB 1725 — passed the House. A modified version passed the Senate, but negotiations to reconcile the two versions were unsuccessful and Medicaid expansion ultimately failed during the 2024 session. The issue of Medicaid expansion is expected to be reconsidered in 2025. 5
2024 was the first year that any Medicaid expansion bill had advanced out of committee in Mississippi, after House Speaker Jason White clarified in the fall of 2023 that Medicaid expansion would be addressed by the legislature in 2024. White noted “I think we as Republicans have probably earned a little bit of the bad rap we get on health care in Mississippi. Part of that is that we haven’t had a full-blown airing or discussion of Medicaid expansion. We’ve just said, ‘No.’” 6
The bill passed by the Mississippi House included a 20-hour-per-week work requirement, but it also noted that if CMS refused to approve the work requirement (as expected under the Biden administration), Medicaid expansion would still take effect from 2025 through early 2029 (a repeal clause in the bill would have ended expansion at that point, unless lawmakers reauthorized it).
But the Senate’s version of the bill included a 30-hour-per-week work requirement and would not have allowed expansion to be implemented if the work requirement wasn’t approved by CMS. That was essentially a poison pill for Medicaid expansion, as it’s expected that the Biden administration will not approve a Medicaid work requirement.
The two chambers worked to reconcile their differences. The Senate offered a version with a 100-hour-per-month work requirement, but still with a clause that would prevent expansion if the federal government didn’t approve the work requirement. The House offered a proposal to put a referendum on the 2024 ballot in Mississippi, asking voters to weigh in on whether Medicaid should be expanded, and if so, whether there should be a work requirement. Senate Republicans were strongly opposed to the ballot referendum proposal, and Mississippi still has no access to citizen-led ballot initiatives. 7 So a citizen-led Medicaid expansion ballot measure cannot be used in Mississippi to expand Medicaid the way several other states have done.
Non-disabled adults without children are not eligible for Medicaid in Mississippi regardless of how low their income is, and parents with dependent children are only eligible with incomes that don’t exceed 24% of the poverty level. This is one of the lowest eligibility caps in the country — only Texas and Alabama have lower limits. 8
If Mississippi did expand eligibility for Medicaid as called for in the ACA, an estimated 220,000 would be newly eligible for coverage. Unfortunately, in the poorest, sickest state in the U.S., the majority of lawmakers and two governors have opted to reject federal funds that would provide health insurance for the state’s poorest residents.
Because Marketplace subsidies are only available in Mississippi for people whose household incomes are at least 100% of poverty, an estimated 74,000 people in Mississippi are in the coverage gap and have no realistic access to health insurance 9 (some analyses indicate that there are more like 130,000 people in the coverage gap in Mississippi). They aren’t eligible for Medicaid, and they also aren’t eligible for subsidies.
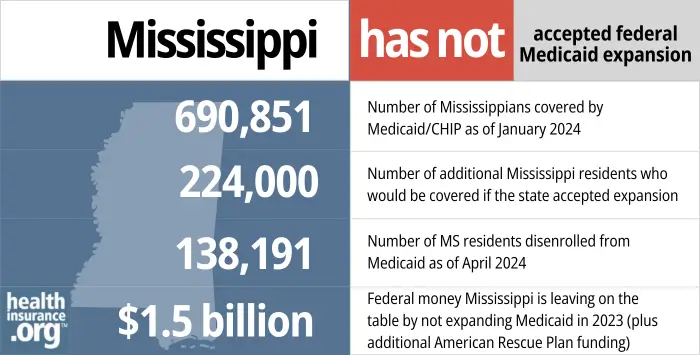 Number of Mississippians covered by Medicaid/CHIP as of January 2024. 224,000 - Number of additional Mississippi residents who would be covered if the state accepted expansion. 138,191 - Number of MS residents disenrolled from Medicaid as of April 2024. ".5 billion - Federal money Mississippi is leaving on the table by not expanding Medicaid in 2023 (plus additional American Rescue Plan funding)." width="700" height="355" />
Number of Mississippians covered by Medicaid/CHIP as of January 2024. 224,000 - Number of additional Mississippi residents who would be covered if the state accepted expansion. 138,191 - Number of MS residents disenrolled from Medicaid as of April 2024. ".5 billion - Federal money Mississippi is leaving on the table by not expanding Medicaid in 2023 (plus additional American Rescue Plan funding)." width="700" height="355" />

Use this guide to help you find the right health plan in Mississippi. Many people find an ACA Marketplace (exchange) plan, also known as Obamacare, to be a cost-effective choice.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Mississippi.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Mississippi as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

If you are under 65 and don’t have Medicare:
If you are 65 or older or have Medicare, use this website to apply for Medicaid.
Many Medicare beneficiaries receive assistance through Medicaid with the cost of Medicare premiums, cost sharing, and services Medicare doesn’t cover — such as long-term care.
Our guide to financial assistance for Medicare beneficiaries in Mississippi explains these benefits, including Medicare Savings Programs, Extra Help, long-term care benefits, and income guidelines for assistance.
Medicaid disenrollments were paused nationwide from March 202o through March 2023. Even if a person’s circumstances changed and they were no longer Medicaid-eligible, their coverage continued throughout the pandemic. Starting in early-mid 2023, states began checking the eligibility of everyone enrolled in Medicaid and disenrolling those who no longer met the eligibility criteria or who failed to respond to a renewal notice.
The first round of disenrollments in Mississippi came in June 2023, By February 2024, 116,705 people had been disenrolled from Mississippi Medicaid. 14 The pace of disenrollments had slowed considerably, with more than 29,000 people disenrolled in June 2023, 15 but fewer than 1,200 disenrolled in December 2023. 16 But more than 6,000 people were disenrolled in February 2024. 17
HealthCare.gov is offering an extended enrollment opportunity, from March 31, 2023 through November 30, 2024, for anyone who loses Medicaid at any time during that window. 18
This means people do not have to enroll within 60 days of losing their Medicaid, as would normally be the case. However, the best course of action is still to enroll as soon as possible, to minimize gaps in coverage (Marketplace plans do not have retroactive effective dates, so a gap in coverage results if you wait to sign up for the new plan until after your Medicaid has ended).
Because Mississippi has not expanded Medicaid under the ACA, the state does still have a coverage gap for adults with income below the poverty level. So it’s important for low-income residents to be aware of how to avoid this coverage gap.
In 2021, Medicaid expansion advocates in Mississippi began gathering signatures to get Initiative 76 on the 2022 ballot. This measure would have let the state’s voters decide whether Medicaid should be expanded, and it’s worth noting that this approach has resulted in Medicaid expansion in several other states — voters have never failed to pass a Medicaid expansion measure in any state when it has been on the ballot.
However, Initiative 76 was suspended in mid-2021, after it was determined that a state Supreme Court ruling in 2020 had invalidated the Mississippi ballot initiative process. So voters in Mississippi did not get a chance to weigh in on Medicaid expansion in the 2022 election.
As noted above, efforts to revive the citizen-led ballot initiative in Mississippi failed in the 2024 legislative session. 7
Even though Mississippi hasn’t expanded Medicaid and has some of the most stringent eligibility guidelines in the country, the state has sought federal approval to make it even harder for people to get Medicaid coverage in Mississippi.
In October 2017, Mississippi submitted a proposed 1115 waiver to CMS, detailing the work requirement that the state wants to implement. The waiver was still pending approval as of 2024, and the Biden administration has informed states that Medicaid work requirements are not compatible with the mission of Medicaid. The Trump administration had approved several states’ proposed Medicaid work requirements, but the Biden administration has revoked all of those approvals. Proposals like Mississippi’s, which were still pending when the Biden administration took office, have been left pending and are unlikely to be approved.
(Georgia implemented a work requirement in 2023, but only for the population that became newly eligible for the state’s partial Medicaid expansion at the same time. The work requirement in Georgia does not apply to anyone who was already eligible for coverage.)
Mississippi’s proposal would allow the state to require some Medicaid enrollees to work, volunteer, attend school, participate in substance abuse treatment, or otherwise fulfill the work requirement for at least 20 hours per week.
People would be exempt if they are disabled, physically or mentally unable to work, a primary caregiver for someone in need of care, elderly, under the age of 19, pregnant, Native American, or included in various other exempt populations. Since Mississippi has not expanded Medicaid under the ACA, the vast majority of the state’s Medicaid enrollees would already be exempt from the work requirement. The work requirement would really only apply to certain low-income parents and people receiving transitional medical assistance (a program that extends Medicaid coverage for up to 12 months for people who start earning too much money to continue to qualify for Medicaid).
Mississippi Medicaid covers about 691,000 people, but only about 56,000 of them are in the low-income parent Medicaid eligibility category. And of those, most would have exemptions. About 15,000 to 20,000 people would end up having to work as a result of the work requirement, and many are already working.
Ultimately, about 5,000 people would be expected to lose coverage in Mississippi each year if the work requirement were to be approved and implemented (as noted above, that is not likely to happen under the Biden administration). According to the Clarion-Ledger, 91% of the people who would lose access to Medicaid under the proposed work requirement in Mississippi are low-income mothers. And more than two-thirds are African American.
These low-income parents are in a catch-22 situation: If they earn more than 27% of the poverty level (that works out to about $518/month for a household of three), they’d no longer be eligible for Medicaid. And if they don’t work, they’ll also lose access to Medicaid as a result of the work requirement. So in order to have health insurance, they would either have to maintain a job that provides health insurance coverage, or earn at least 100% of the poverty level so that they could obtain premium subsidies in the exchange and purchase an affordable individual health plan. One hundred percent of the poverty level is about $1,919/month for a household of three, so it’s a big jump from the Medicaid eligibility cutoff to the start of eligibility for premium subsidies.
To address these concerns, the state proposed an additional 12 months of transitional Medicaid coverage for people who remain in compliance with the work requirement for the full 24 months. Georgetown University’s Joan Alker describes this as a “wholly inadequate solution.” It’s temporary, doesn’t provide any sort of solution after the 24 months of transitional Medicaid coverage ends, and hinges on the unrealistic expectation that low-income, working parents will not experience even one month of unemployment during their 24 months of transitional Medicaid.
CMS had initially opened a comment period in early 2018 for Mississippi’s waiver proposal. But after the state revised the proposal to add 12 months of transitional Medicaid coverage, the comment period was re-opened. During the re-opened comment period, 320 comments were submitted, and 319 of them were in opposition to the state’s proposed Medicaid work requirement. The revised proposal is still under review by CMS as of 2024, but is unlikely to ever be approved.
Total Mississippi Medicaid/CHIP enrollment was 690,851 as of January 2024, 19 including 610,448 people with Medicaid and 80,403 children with health insurance coverage under CHIP.
Total enrollment was 12% higher as of January 2024 than it had been in late 2013. 20 The growth was largely due to the COVID pandemic, and enrollment began declining in mid-2023, after the pandemic-related continuous coverage rule ended (details above).
As the ACA was written, it called for Medicaid expansion in every state for residents with incomes up to 133% of poverty (plus a 5% income disregard, bringing the effective eligibility threshold to 138% of the poverty level). But in 2012, the Supreme Court ruled that states could not be penalized for opting out of expansion, and Mississippi is one of only ten states that have not yet expanded Medicaid.
In states that expand Medicaid, the federal government paid the full cost of expansion through 2016. After that, states gradually began to pay a share of the expansion cost, but the federal government will always pay at least 90%. As a result, states that reject Medicaid expansion are leaving billions of dollars on the table.
From 2013 through 2022, Mississippi gave up $14.5 billion in federal funding that would otherwise have been available to the state to help provide medical care for low-income residents. And states that newly expand Medicaid after April 2021 are eligible for two years of additional federal Medicaid funding under the American Rescue Plan, but Mississippi has not yet taken advantage of that.
Since residents in states not expanding Medicaid still have to pay federal taxes, Mississippi residents have been subsidizing Medicaid expansion in other states. Over a decade, people in Mississippi are paying $1.7 billion in federal taxes that are used to pay for Medicaid expansion in other states.
Governor Tate Reeves, who assumed office in 2020, campaigned in opposition to Medicaid expansion. His viewpoint is consistent with former Governor Phil Bryant. Bryant claimed that the state wouldn’t be able to bear the cost if the federal government were ever unable to uphold its promise to pay at least 90% of the cost, and referred to accepting Medicaid expansion as a “fool’s errand.”
Mississippi’s share of traditional Medicaid costs climbed from fiscal year 2012 to fiscal year 2017. Lawmakers have highlighted this as a reason for not expanding coverage, but they’re missing the point (whether purposely or not) that Medicaid expansion is funded under different rules from traditional Medicaid. Under Medicaid expansion, the cost to cover newly eligible residents was fully funded by the federal government through the end of 2016. In 2020 and forward, states pay 10% of costs associated with the Medicaid expansion population.
And of particular importance, states that have expanded Medicaid have seen substantially smaller growth in state Medicaid spending than states that haven’t expanded Medicaid.
In June 2013, Republicans in both chambers of the Mississippi legislature voted against Medicaid expansion. They did vote to continue the state’s existing Medicaid program, which came within days of expiring and had to be dealt with in a special legislative session called by Bryant. The issue of Medicaid expansion might not have even made it to a vote except that Democrats threatened to withhold their votes for renewing the existing Medicaid program unless Republicans would agree to take the issue of Medicaid expansion to a vote. No Republicans voted for Medicaid expansion, although one, Senator Billy Hudson of Hattiesburg, said that he would eventually vote for Medicaid expansion, “but not today.”
The Mississippi State Medical Association put forth a resolution in August 2016 calling for “expanded coverage” but didn’t use the words “Medicaid expansion” in their draft, knowing that the issue was too politically charged.
As described above, Mississippi lawmakers finally considered Medicaid expansion during the 2024 legislative session, but were unable to come to an agreement. The issue is expected to be considered again in 2025. But for now, in the nation’s poorest state, the poorest residents have no access to health coverage at all.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.